Implications for Human-Centric Lighting Design in Tropical Nursing Homes: A Pilot Study
Light synchronizes our physiological and psychological rhythms to the 24-hour rhythm of the ambient changes. For the elderly, adequate environments to compensate for increasing frailty and sensory loss are crucial. Dr. Szu-Cheng Chien, Assistant Professor at the Singapore Institute of Technology reports from a pilot study that aimed to explore HCL design strategies in nursing homes in Singapore. Pre-/post implementation user surveys and quantitative evaluations were conducted.
For the elderly, an adequate environment to compensate for increasing frailty and sensory loss are crucial. Normal, age-related changes to the eyes decrease the amount of light that reaches the retina, impacting both vision and circadian rhythm. Some attempts have been made recently to conduct white-tunable lighting and vary lighting levels and CCT for health and wellness. However, how to translate such Human-centric Lighting (HCL) concepts proven in laboratory studies into built environments are still in the early stage and lack largely proven practices and strategies on an operational level. This research project aimed to explore HCL design strategies in nursing homes in Singapore. Firstly, state of the art HCL and aging studies were discussed. We then captured the views to illustrate an HCL framework in a tropical context, whereby the quantitative and qualitative approaches were considered. The preliminary design strategies were developed based on this framework and exemplified in a selected nursing home in Singapore. Also, pre-/post implementation user surveys together with quantitative evaluations (involving horizontal and corneal illuminance measurements) were conducted for assessing the performance of the HCL design strategies. These pilot study findings provide initial insight into HCL design-related knowledge and serve as the solid basis towards the HCL best practices in the environment of nursing homes in Singapore.
Introduction
While typical nursing homes provide insufficient lighting, nursing home residents with greater visual impairment perceive far less bright light exposure for circadian rhythm. That leads to the increase of residents' falls, hip fractures, daytime behavior and sleep problems, etc. Nonetheless, how to translate the HCL concepts proven in laboratory studies into built environments, including hospitals and nursing homes, are still in the early stage and lack of largely proven practices and strategies on an operational level. Specifically, the necessary requirements for the development and effectiveness of control system for HCL in nursing homes have not been formulated in a rigorous and reliable manner.
To date, the designs of lighting systems in nursing homes are primarily made to support visual acuity for staff and secondly to minimize hazards such as staircases. However, to obtain proper visual sharpness and better contrast people of older age require heightened light levels due to age-related failing vision. Furthermore, the nursing home environments are often purpose- made for hygiene, cleanliness and safety and ignore that light sources produce substantial glare due to shiny floors/surfaces and inappropriate light at night disrupts not only sleep but also the timing of the body clock, with negative consequences for cognition and emotions. Properties of current lighting systems are inflexible and not designed to take non-visual effects of light into account for older people's wellbeing in nursing homes.
In the last two decades, much has been learned regarding the non-visual effects of light on human circadian entrainment. Light synchronizes physiological and psychological rhythms to the 24-hour rhythm of the environment [1,2]. Light has also acute alerting and activating effects [3], can affect mood [4], and, when applied at night, suppresses melatonin production [5]. These are some examples of the non-visual effects of light in humans. Studies of the biological clock have shown a reduced neuronal activity in the SCN of the elderly, especially after the age of 80 [6], and reduced circadian rhythm amplitude after the age of 50 [7]. This suggests that, at a molecular level, the SCN becomes less responsive to entrainment stimuli such as light-induced neural signals from the retina. Further, it is suggested that some of the neural processes involved in the entrainment process might be dysfunctional or less effective as we age [8]. Thus, the elderly (specifically those with dementia) commonly suffer from mental and behavioral disorders, such as sleep disturbances, agitated behavior, depression, and risk of falls. Studies [9-16] have shown that light therapy supported by professional lighting control system can effectively offset these issues and add to the quality of life (e.g., consolidate rest/activity patterns, improve sleep efficiency, cognition, reduce symptoms of depression and alter the levels of aggressive behaviors) to the elderly with dementia in spatial and temporal dimensions.
How to translate the HCL concepts proven in laboratory studies into system implementation in real built environments, including hospitals and nursing homes, are still in the early stages and lack largely proven practices and strategies on an operational level [17,18]. There are a few past and ongoing pilot research and development efforts that have partially addressed certain aspects of the concerns of this current proposal. Such precedents include "Rigshospitalet, Psychiatric Centre Copenhagen: Research project on Ergonomic Circadian Lighting in psychiatry" [19], "Gateway- evaluating a trial LED Lighting System at the ACC Care Center in Sacramento, CA" [20], "Elderly Care Home in Solingen Germany" [21], and "Improved quality of life for resident dementia patients: St. Katharina research project in Vienna" [22]. In these projects, companies in lighting industry (e.g., OSRAM, Philips Lighting, Zumtobel) worked closely with the academia and healthcare institutes.
In this study, we aim to develop and implement a set of advanced human-centric lighting control strategies to improve the comfort and care of seniors, assist the nursing staff in their nightly rounds, and help residents navigate facility hallways via customizing light exposure scenarios for the residents and staffs.
Approach
Description of the case study area
This pilot study was conducted in a selected residence at level one of the Salvation Army Peacehaven Nursing Homes in Singapore. This residence is an entry-controlled area with natural ventilation, including 3 six-bedded rooms, 3 single-bedded rooms, 1 activity room, 8 toilets, and corridor (Figure 3). There are 21 senior residents with mild dementia residing in this home. In this residence, the lighting system will be retrofitted from conventional 24W CFL lamps with fixed CCT level (i.e., 4700 K) to 10W advanced tunable-white LED (2700 K to 5000 K; UGR<19; beam angle 40°) (Figure 3). In addition, the smart lighting control system has been installed to allow for individual luminaire control by mobile app via Bluetooth-based mesh network.
 Figure 2: The previous and selected luminaires for retrofitting
Figure 2: The previous and selected luminaires for retrofitting
Pre-implementation assessment
This step includes pre-implementation user survey, on-site illuminance measurement of original lighting performance for the above-mentioned spaces, namely bedded rooms, corridor, activity room, and toilet. Nursing staff (14 females and 1 male, average age: 35.4 years, average working period of 8.11 years in this nursing home) were selected as participants to provide their feedback and investigate the residents' perception variables based on the observation from 15 March to 15 May 2017. The user survey with was conducted in from 15 to 30 May, 2017. Based on the above-mentioned assessments, the conceptual design of the control strategies together with user scenarios was developed. The questionnaires for pre-/post implementations was approved by the IRBs of Singapore Institute of technology and the Salvation Army Peacehaven Nursing Home. We selected 7 locations as reference points for the session of on-site measurements. Also, the illuminance meter (Gossen Mavolux 5032) was used to measure the illuminance in selected reference points.
Benchmarking of available strategies
This step addresses the benchmarking of available strategies in view of different space categories through the lighting simulation tool, ElumTools, as a plugin of Autodesk Revit. Such considered spaces include corridor, single/6-bedded rooms, and activity room. The preliminary simulations were conducted to compare the visual performances of the scenarios with existing CFL and the ones with selected tunable-white luminaires.
Human-centric lighting implementation and fine-tuning
This step includes the installation of the advanced tunable LED luminaire control system in the selected site. This system comprises IoT-based tunable LED luminaires with plug-and-play capability, user-friendly interface (involving embedded multiple control interface in smart devices and the re-use of wall switch), and advanced sensing technologies (e.g., human motion, movement direction, motionless occupancy, fallen human detection, high temperature). Also, preliminary human centric lighting strategies were implemented, tested, and commissioned (Figure 3). The installation and commissioning period was from 1 June to 15 August 2018. After this step, the settings with new control strategies were operated for two months, from 15 August to 15 October.
![Figure 3: The control scenarios involving luminance output and CCT appearance in the bedded rooms [A], the activity room [B], the corridor [C], and the toilets [D] Figure 3: The control scenarios involving luminance output and CCT appearance in the bedded rooms [A], the activity room [B], the corridor [C], and the toilets [D]](https://www.led-professional.com/media/resources-1_articles_implications-for-human-centric-lighting-design-in-tropical-nursing-homes-a-pilot-study_figure-3.jpg/@@images/image-1280-c6db98745ed572e468e6b01995aec3ed.jpeg) Figure 3: The control scenarios involving luminance output and CCT appearance in the bedded rooms [A], the activity room [B], the corridor [C], and the toilets [D]
Figure 3: The control scenarios involving luminance output and CCT appearance in the bedded rooms [A], the activity room [B], the corridor [C], and the toilets [D]
Post-implementation assessment
In this step, we verified and validated the performance of the human centric lighting strategies via post-implementation user surveys.
The previous-selected (total of 15) nursing staff, as participants, conducted the user surveys again to provide their feedback and investigate the residents' perception variables in view of visual comfort level of the residents and staff based on the observation during the operation period. The user survey was conducted from 15 to 31 October, 2017. We also measured the illuminance level in 7 selected reference points via the illuminance meter (Gossen Mavolux 5032).
Data Analysis and Discussion
In this step, we analyzed the collected survey data and discussed the results.
Results
The data analysis involved:
• preliminary simulation-based evaluation,
• on-site illuminance comparison based on pre-/post retrofitting,
• Data analysis based on pre-/post installations user questionnaires
Preliminary simulation-based evaluation
The BIM model of the selected residence was built in Autodesk Revit for carrying out a set of simulation with its advanced lighting plugin, ElumTools. Specifically, we evaluated the results of selected areas for further assessment, namely one six bedded room, one toilet, the corridor and activity room. Figure 4 and Figure 5 illustrates an example of the simulation results pertaining to illuminance distributions of existing CFL luminaire and proposed retrofitted LED with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700 K at the floor and reading levels (0 cm and 85 cm) in selected six-bedded room and the corridor. The results suggest that the proposed retrofitted tunable-white LED has a significant visual performance with higher uniformity compared with the pre-installation scenario.
![Figure 4: A set of simulation results involving the pre-implementation scenario [A] and four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the floor level (0 cm), namely [B], [C], [D], [E]; unit: lx Figure 4: A set of simulation results involving the pre-implementation scenario [A] and four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the floor level (0 cm), namely [B], [C], [D], [E]; unit: lx](https://www.led-professional.com/media/resources-1_articles_implications-for-human-centric-lighting-design-in-tropical-nursing-homes-a-pilot-study_figure-4.jpg/@@images/image-1280-c6db98745ed572e468e6b01995aec3ed.jpeg) Figure 4: A set of simulation results involving the pre-implementation scenario [A] and four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the floor level (0 cm), namely [B], [C], [D], [E]; unit: lx
Figure 4: A set of simulation results involving the pre-implementation scenario [A] and four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the floor level (0 cm), namely [B], [C], [D], [E]; unit: lx
![Figure 5: A set of simulation results involving four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the reading level (85 cm), namely [A], [B], [C], [D]; unit: lx Figure 5: A set of simulation results involving four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the reading level (85 cm), namely [A], [B], [C], [D]; unit: lx](https://www.led-professional.com/media/resources-1_articles_implications-for-human-centric-lighting-design-in-tropical-nursing-homes-a-pilot-study_figure-5.jpg/@@images/image-1280-c6db98745ed572e468e6b01995aec3ed.jpeg) Figure 5: A set of simulation results involving four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the reading level (85 cm), namely [A], [B], [C], [D]; unit: lx
Figure 5: A set of simulation results involving four sets of post-implementation scenarios with four levels (i.e., 100, 50, 30, 10 percent) and CCT value 2700K at the reading level (85 cm), namely [A], [B], [C], [D]; unit: lx
On-site illuminance comparison
In this section, we compared the illuminance measurement data between pre/post- installation scenarios in this residence. As previously mentioned, we have selected two reference points in one six-bedded room (B1, B2), two points in the corridor (C1, C2), two points in the activity room (A1 and A2), and one point in the selected toilet (T1) (Figure 6). The comparison results are arranged in following tables in accordance with the previously described spaces, namely bedded room, toilet (Table 1), corridor, and activity room (Table 2).
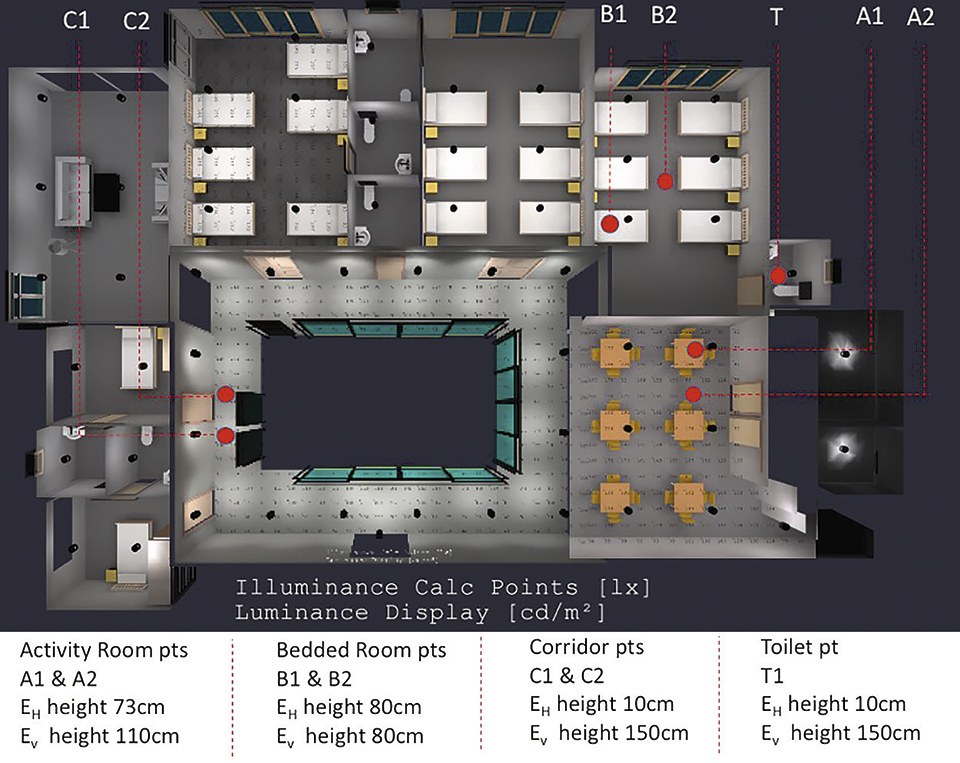 Figure 6: The locations of the measurement points with height information
Figure 6: The locations of the measurement points with height information
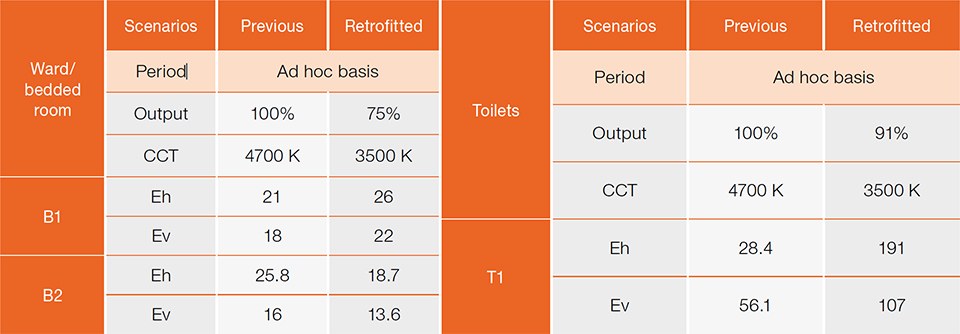 Table 1: Measurement results in the bedded Rooms and toilets; unit: lx
Table 1: Measurement results in the bedded Rooms and toilets; unit: lx
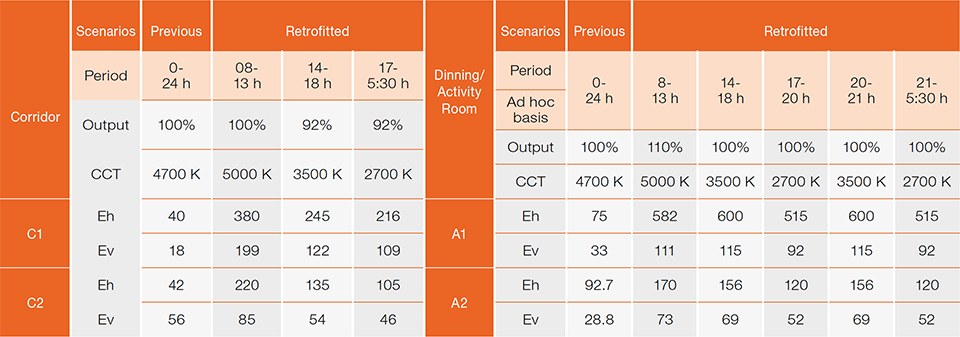 Table 2: Measurement results in the corridor, and activity room; unit: lx
Table 2: Measurement results in the corridor, and activity room; unit: lx
Data analysis
The results of the above-mentioned sessions (i.e., Section 5 and 5) involving 15 participants were analyzed in terms of three categories.
The categories pertain to:
• Lighting experiences
• Feedback
• Investigation of the residents' perception variables in temporal
(i.e., day and night) and spatial (involving bedded room, corridor, toilet,
and activity room) approach based on their observation.
Thereby, the five-point qualitative Likert scale of the questionnaire was further converted to numerical values (from 1 to 5). Initial results of the analysis if these sessions are given in the following figures as mean values. In addition, we conducted a two-tailed t-test to better evaluate the significant difference between pre and post-retrofitting data. Figure 7 (mean values) compares the evaluation results regarding their lighting experiences in bedded rooms. As the results shown in figure 7 imply, HCL solution in our study provides the participants with significantly pleasant lighting experiences in a bedded room. HCL solution fairs better than CFL in terms of the categories of natural and bright lighting experiences. Figure 8 shows a comparison of theirs' and residents' (via observation) perceptual attitudes in bedded rooms. As the results shown in figure 8 imply, the residents are slightly easier to move around during the night. Also, the residents slightly prefer warm white for the color appearance of the lighting in a bedded room during the night. The nursing staff are slightly more satisfied with the visual environment at night.
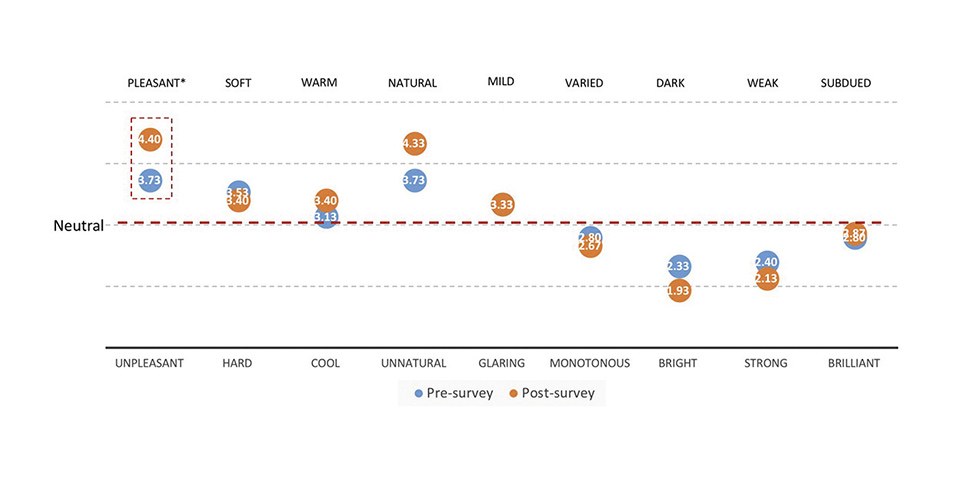 Figure 7: Light experience in the bedded rooms (Mean values, N=15); *p<0.05
Figure 7: Light experience in the bedded rooms (Mean values, N=15); *p<0.05
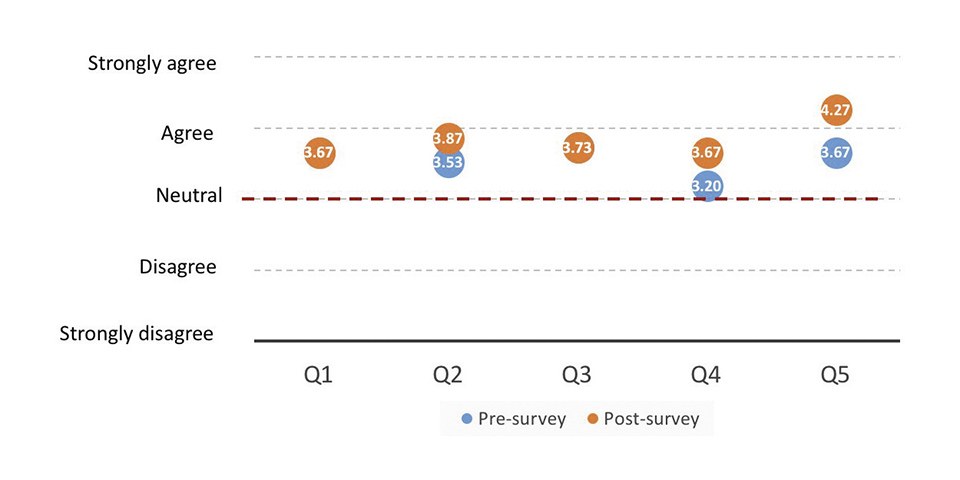 Figure 8: Evaluation results related to the perceptual attitudes in the bedded rooms (Mean values, N=15)
Figure 8: Evaluation results related to the perceptual attitudes in the bedded rooms (Mean values, N=15)
Figure 9 and figure 10 compare the results involving lighting experiences perceptual attitudes in the corridor while Figure 11 and Figure 12 do the same for the activity room. As the results shown in figure 9 imply, HCL solution in our study provides the participants with significantly natural and strong lighting experiences in the corridor. HCL solution in our study provides more pleasant and bright lighting experiences in the corridor. The results show that staff and residents both have AGREE ratings regarding the sufficient and uniformed brightness of the lighting during the day and night. As the results shown in figure 10 indicate, the residents and staffs significantly prefer cool white in the corridor during the day. Also, residents slightly prefer warm white during the night while the staff significantly prefer warm white during the night. As the results shown in figure 11 imply, HCL solution provides the participants with significantly more monotonous lighting experiences in activity/dining room. HCL solution fairs better than CFL in terms of the categories of natural lighting experiences. As the results shown in figure 12 imply, the staff significantly prefer warm white for the color appearance of the lighting in the activity room during the night while the residents remain neutral. The residents are slightly more comfortable with light conditions in activity room throughout the whole day. The residents slightly prefer cooler white during the day. No significant difference for task performance of residents during the day and caregivers during the night. Figure 13 related to the comparison of their and residents' (via observation) perceptual attitudes in the toilet. The participants left AGREE ratings in terms of the clear path to the toilet due to the sufficient brightness of the HCL lamps throughout the whole day. The participants are with neutral rating in terms of warm white for the color appearance of the lighting in the toilet during the night. As the results shown in figure 13 portray, the residents significantly prefer cool white for the color appearance of the lighting in the toilet during the day. Also, the glare has been slightly restrained.
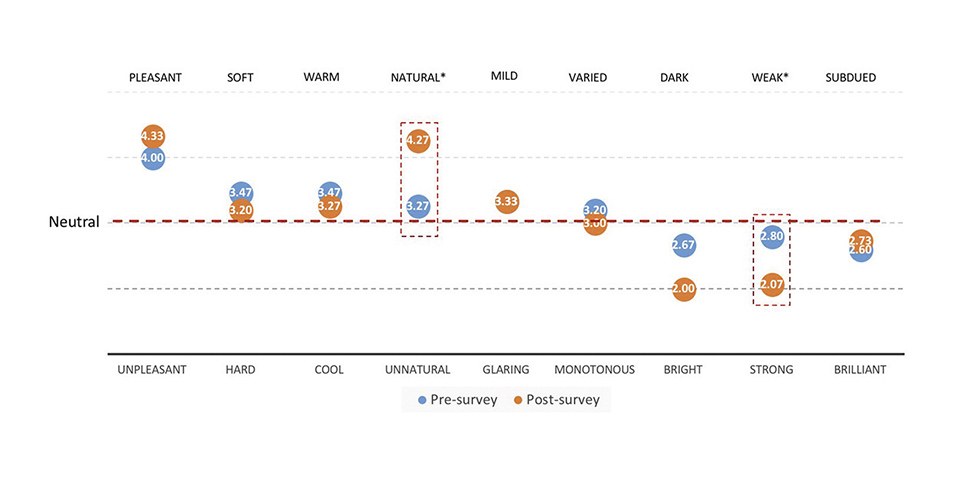 Figure 9: Light experience in the corridor (Mean values, N=15); *p<0.05
Figure 9: Light experience in the corridor (Mean values, N=15); *p<0.05
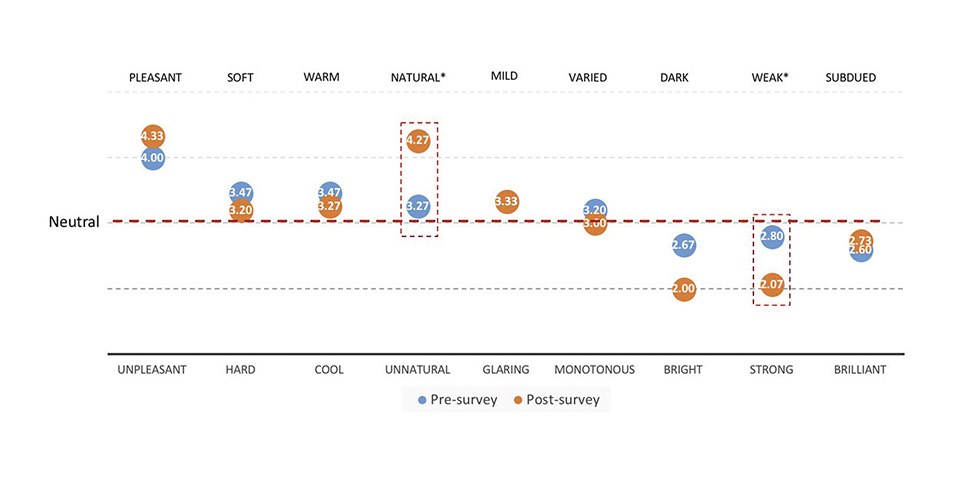 Figure 10: Evaluation results related to the perceptual attitudes in the corridor (Mean values, N=15); *p<0.05
Figure 10: Evaluation results related to the perceptual attitudes in the corridor (Mean values, N=15); *p<0.05
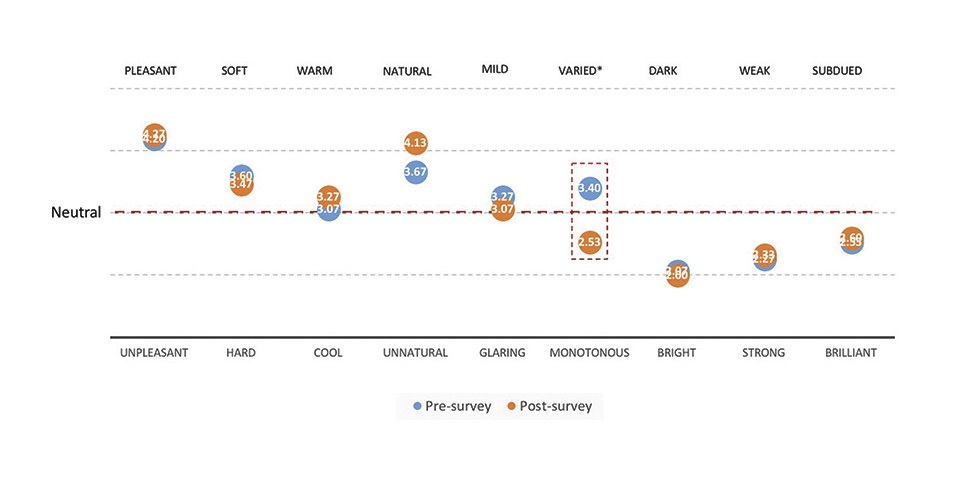 Figure 11: Light experience in the activity room (Mean values, N=15); *p<0.05
Figure 11: Light experience in the activity room (Mean values, N=15); *p<0.05
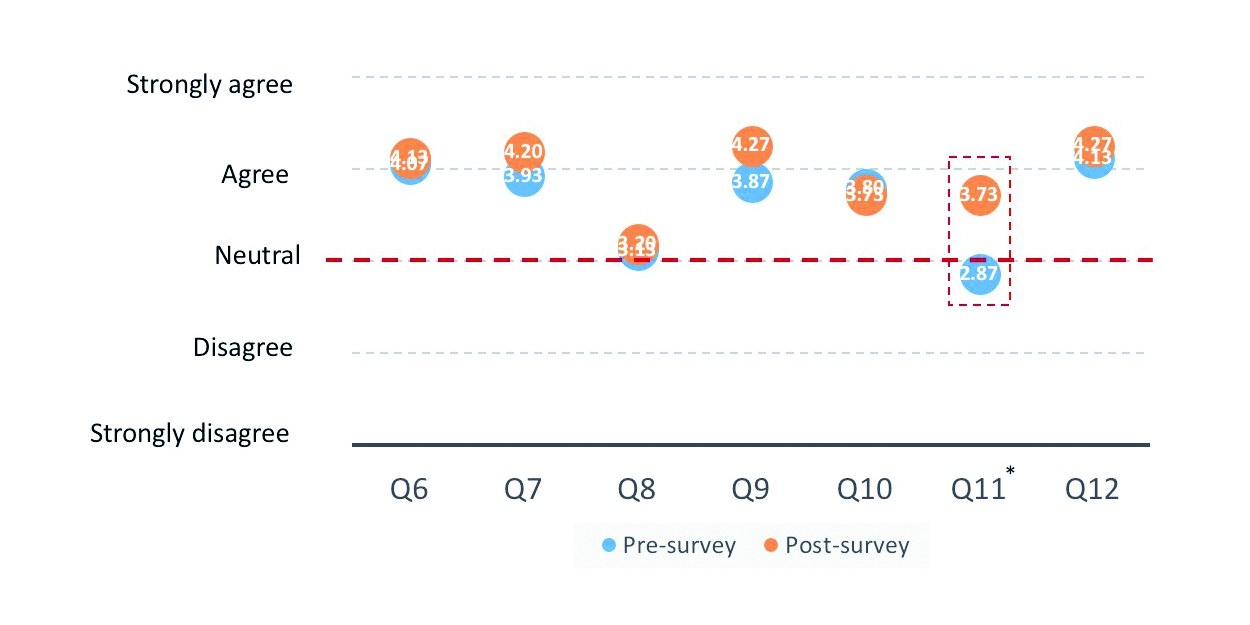 Figure 12: Evaluation results related to the perceptual attitudes in the activity room (Mean values, N=15); *p<0.05
Figure 12: Evaluation results related to the perceptual attitudes in the activity room (Mean values, N=15); *p<0.05
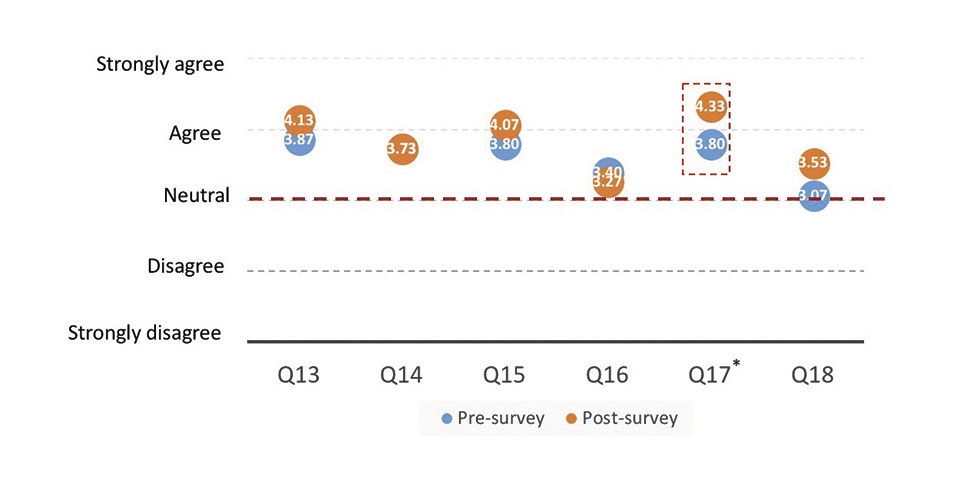 Figure 13: Evaluation results related to the perceptual attitudes in the toilet (Mean values, N=15); *p<0.05
Figure 13: Evaluation results related to the perceptual attitudes in the toilet (Mean values, N=15); *p<0.05
Limitations
In our research efforts, computational lighting simulations and empirical measurements were successfully applied for the comparative studies. However, the results could be further compared for all the spaces instead of selected rooms and reference points. Also, in order to better evaluate the impacts of HCL lighting, the supplementary data (involving the body health) of the senior with mild dementia collected via FDA-approved wearable devices could be included in future studies.
Concluding Remarks
As the regular circadian rhythm is timely required for those seniors with mild dementia and nursing staff with long-term working hours, it is necessary to specify the circadian practices in the nursing homes based on our findings in previous sections, whereby two primary focus strategies are discussed below. Firstly, the effective methods to maintain the circadian rhythm should be further explored. Such an example includes the optimization of natural light levels with the replacement and/or supplement of electric lighting to artificially stimulate the human circadian system. Thus, the natural light and dark cycles are enhanced to facilitate sleep while natural light spectrum shift with the supplement of artificial lighting over the 24 hours are conducted. Potential applicable spaces in the nursing homes include ward bedded rooms, non-work related windowless environments, common areas, communal environments where relaxation is emphasized. In addition, for gloomy spaces with poor daylight penetration, advanced dynamic lighting control systems could be applied to artificially emulate a cycle of dynamic light with natural color shifts timed for circadian support. Also, it may be applied to provide tunable wavelengths of enhanced blue or white light for the purpose of enhancing performance and eliciting specific behavioral outcomes. Potential applicable spaces in nursing homes comprise nursing stations, dispensing pharmacy point, windowless office environments, night shift work areas, and residential settings for better sleep quality management.
These research efforts contributed to the above-mentioned two focus strategies. The presented paper demonstrated the preliminary study of a design strategy for HCL systems in nursing homes. Firstly, state of the art HCL and aging studies were discussed. We then captured the views to illustrate the preliminary HCL design strategies in a tropical nursing home, whereby the quantitative and qualitative approaches were considered. The preliminary design strategies were developed and exemplified in a selected nursing home in Singapore. Also, pre-/post implementation user surveys together with quantitative evaluations (involving horizontal and corneal illuminance measurements) were conducted for assessing the performance of the HCL design strategies. These pilot study findings provide initial insight into HCL design-related knowledge and serve as the solid basis towards the HCL best practices in the environment of nursing home in Singapore. For future phases of this research, we will try to further articulate current effort toward the implementation of HCL for a diversity of space and building types in the Tropics.
Appendix:
Questions related to the perceptual attitudes in the questionnaire:
Q1: The residents are able to fall asleep within 30 minutes in the bedded
room during the night in the past month
Q2: The residents are able to move about with ease during the night
Q3: The residents feel safe to move about with the lighting levels during
the night
Q4: The residents prefer warm white for the color appearance of the
lighting in the bedded room during the night
Q5: You are able to work with ease attending to the residents with the
lighting during the night
Q6: The residents can easily perform their tasks with the light conditions in
the activity room during the day
Q7: The residents are comfortable with the light conditions in the activity
room throughout the whole day
Q8: The residents prefer warm white for the color appearance of the
lighting in the activity room during the night
Q9: The residents prefer cool white for the color appearance of the lighting
in the activity room during the day
Q10: You are able to provide care to the residents in the activity room with
current light condition during the night
Q11: You prefer warm white for the color appearance of the lighting in the
activity room during the night
Q12: You prefer cool white for the color appearance of the lighting in the
activity room during the day
Q13: The residents can see the path to the toilet during the night
Q14: The lamps provide sufficient and uniformed brightness for the
residents in the toilets during the night
Q15: The lamps provide sufficient and uniformed brightness for the
residents in the toilets during the day
Q16: The residents prefer warm white for the color appearance of the
lighting in the toilet during the night
Q17: The residents prefer cool white for the color appearance of the lighting
in the toilet during the day
Q18: The mirrors and tiles do not cause blinding glare (by reflection)
throughout the whole day
Q19: The lamps provide sufficient and uniformed brightness for the
residents in the corridor during the day
Q20: The residents prefer cool white for the color appearance of the lighting
in the corridor during the day
Q21: The lamps provide sufficient and uniformed brightness for the
residents in the corridor during the night
Q22: The residents prefer warm white for the color appearance of the
lighting in the corridor during the night
Q23: The lamps provide sufficient and uniformed brightness for you in the
corridor during the day
Q24: You prefer cool white for the color appearance of the lighting in the
corridor during the day
Q25: The lamps provide sufficient and uniformed brightness for you in the
corridor during the night
Q26: You prefer warm white for the color appearance of the lighting in the
corridor during the night
Q27: There is little distracting reflection and glare is in the corridor
Acknowledgment:
The research presented in this paper is supported in part by in-kind contributions from Singapore Green Building Council (SGBC), Photizo Global Pte Ltd, and Singapore Institute of Technologies. Authors gratefully acknowledge the support of Prof. Tseng King Jet, Asscoc. Prof. Rosy TAY, Dr. Davy Cheung, and Mr. Christopher Lee toward the completion of this research efforts in this paper.
References:
[1] Rea M.S. and Figueiro M.G. (2016). "Light as a circadian stimulus for
architectural lighting". Lighting Res. Technol. 2016;0:1-14
[2] Lucas R. J., Peirson S.N., Bersons D. M., Brownl T. M., Cooper H. M.,
Czeisler C.A., Figueiro M.G., Gamlin P.D., Lockley S. W., O'Hagan J.B.,
Price L.L. A., Provencio I., Skene D.J.,and Brainard G.C. (2014)
"Measuring and using light in the melanopsin age", Trends Neurosci.
37(1): 1–9
[3] Cajochen C. (2007). "Alerting effects of light". Sleep Med Rev.
11(6):453–64
[4] Burkhalter, H.; Wirz-Justice, A.; Denhaerynck, K.; Fehr, T.; Steiger, J.;
Venzin, R. M.; Cajochen, C.; Weaver, T. E.; Geest, S. De. (2015).
"The effect of bright light therapy on sleep and circadian rhythms in
renal transplant recipients: a pilot randomized, multicentre wait-list
controlled trial", In Transpl Int., doi: 10.1111/tri.12443, volume 28(1), 2015
[5] Lewy, A. J., Sack, R. L. and Singer, C. L. (1984). "Assessment of
treatment of chronobiologic disorders using plasma melatonin levels
and bright light exposure: the clock-gate model and the phase
response curve". Psychopharmacol. Bull., 20: 561–565
[6] Swaab D, Fliers E, Partiman T. The suprachiasmatic nucleus of the
human brain in relation to sex, age and senile dementia. Brain Res.
1985;342:37–44
[7] Hofman MA, Swaab DF. Living by the clock: the circadian pacemaker in
older people. Ageing Res Rev. 2006;5:33–51
[8] Skene DJ, Swaab DF. Melatonin rhythmicity: effect of age and
Alzheimer's disease. Exp Gerontol. 2003;38:199–206
[9] Lieverse R1, Van Someren EJ, Nielen MM, Uitdehaag BM, Smit JH,
Hoogendijk WJ. (2011). "Bright light treatment in elderly patients with
nonseasonal major depressive disorder: a randomized placebo-
controlled trial". Arch Gen Psychiatry. 68(1):61–70
[10] Hanforda N. and Figueiro M. (2013). "Light Therapy and Alzheimer's
Disease and Related Dementia: Past, Present, and Future",
J Alzheimers Dis. 33(4): 913–922
[11] Alessi CA, Martin JL, Webber AP, Cynthia Kim E, Josephson KR.
Randomized, controlled trial of a nonpharmacological intervention to
improve abnormal sleep/wake patterns in nursing home residents.
J Am Geriatr Soc. 2005;53:803–810
[12] Ancoli-Israel S, Gehrman P, Martin JL, Shochat T, Marler M,
Corey-Bloom J, Levi L. Increased light exposure consolidates sleep and
strengthens circadian rhythms in severe Alzheimer's disease patients.
Behav Sleep Med. 2003;1:22–36
[13] Burns A, Allen H, Tomenson B, Duignan D, Byrne J. Bright light therapy
for agitation in dementia: a randomized controlled trial.
Int Psychogeriatrics. 2007;21:711
[14] Lovell BB, Ancoli-Israel S, Gevirtz R. Effect of bright light treatment on
agitated behavior in institutionalized elderly subjects. Psychiatry Res.
1995;57:7–12
[15] Hickman SE, Barrick AL, Williams CS, Zimmerman S, Connell BR,
Preisser JS, Mitchell CM, Sloane PD. The effect of ambient bright light
therapy on depressive symptoms in persons with dementia.
J Am Geriatr Soc. 2007;55:1817–1824
[16] Figueiro MG, Gras LZ, Rea MS, Plitnick B, Rea MS. Lighting for
improving balance in older adults with and without risk for falls.
Age Ageing. 2012;41:392–395
[17] Halper M. (2016). "Human-centric lighting set to drastically improve
workplace and individual performance". LEDs Magazine. (Oct 2016). 49–54
[18] Konis K. (2017). "A novel circadian daylight metric for building design
and evaluation". Building and Environment. 113(2017). 22–38
[19] Chromaviso. Research in Circadian Lighting and user evidens.
http://chromaviso.com/en/ergonomiccircadian- lighting/research-in-circadianlighting/ (20 April 2017, date last accessed)
[20] DOE. Gateway- evaluating a trial LED Lighting System at the ACC
Care Center in Sacramento, CA. https://energy.gov/sites/prod/files/2016/ 09/f33/2016_gateway-acc.pdf. (20 April 2017, date last accessed)
[21] Philips Lighting. Elderly Care Home in Solingen Germany.
http://www.lighting.philips.com.sg/ cases/cases/healthcare/elderly-care-home.
(20 April 2017, date last accessed)
[22] Zumtobel. Improved quality of life for resident dementia patients:
St. Katharina research project in Vienna. http://www.zumtobel.com/PDB/teaser/EN/ Study_Health_and_Care_StKatharina.pdf.
(20 April 2017, date last accessed)

